Read the first part of this article as published in the 2013 DINET newsletter.
Part II: Observations, Findings and Recommendations Create Hope For the Future
During a physician-patient small group discussion at last year’s Mastocytosis Society Conference, the question was raised, “How many of you have been diagnosed with POTS?” (Postural OrthostaticTachycardia Syndrome). Surprisingly, approximately half of the group, approximately 20 out of 40 patients raised their hands. POTS is a chronic form of dysautonomia characterized by tachycardia in response to orthostatic stress such as going from a sitting position to standing and may involved multiple organ systems. The symptoms can range in severity from mild to disabling. Interestingly, the co-existing conditions of dysautonomia did not stop with POTS. Patient participants reported diagnoses with other forms of dysautonomia including Neurally Mediated Syncope (NMS, also known as Neurocardiogenic Syncope or Vasovagal Syncope), and Orthostatic Hypotension. Interestingly, the coexisting mast cell disorders included patients with disorders along the mast cell activation disorder spectrum (MCAD) including IgE-mediated Anaphylaxis, Cutaneous Mastocytosis, Systemic Mastocytosis, and Mast Cell Activation Syndrome (MCAS). Clearly, there appears to be a connection between dysautonomia and mast cell activation (MCA), but what? The presence of gastrointestinal (GI) symptoms may be prominent in both of these disorders but in general, the involvement of mast cell mediator activity and its association with ANS dysfunction is a topic that has been given little attention. Further study in this area may provide clues about the pathophysiology of both dysautonomia and MCADs.
OBSERVATIONS
It is known that mast cells interact closely with nerves. Mast cells have been observed degranulating adjacent to nerve synapses and increased numbers of activated mast cells have been documented in the mucosal tissues in “functional” gastrointestinal (GI) disorders that often coexist with dysautonomia. It therefore makes sense that abnormal mast cell mediator release may be a driving force behind nervous system disorders that involve the ANS and that may lead to GI symptoms. The ANS is made up of three parts: the sympathetic nervous system, the parasympathetic nervous system and the enteric nervous system (ENS). Much of the current study of dysautonomia focuses on the roles of the sympathetic and parasympathetic nervous systems, however there has been little emphasis on the ENS. The ENS is comprised of a fabric-like system of neurons that are located in the smooth muscle linings of the intestines (see figure below) and plays in important role in many GI functions. It stands to reason that dysautonomia affecting the ENS leads to GI symptoms.
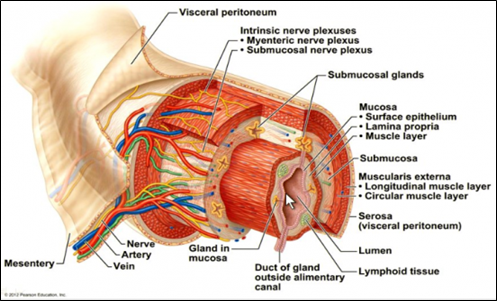
This cutout view of the small intestine illustrates the location of the nerves that make up the ENS.
Basic structure of the alimentary canal, including its four basic layers. Digital illustration. © 2012 Pearson Education, Inc.
<www.anatomyandphysiologyi.com/digestive-system-histology-alimentary-canal/>
Not enough is known about MCA. However, it may be one of the more important medical findings of our time. There are many theories about the basic mechanisms of MCA that may contribute to GI symptoms including diarrhea and abdominal pain. For example, mast cells may activate near the nerve synapses in the smooth muscle walls surrounding the lining layers of the GI tract possibly changing the “leakiness” of the gut. At this time there is not enough clinical evidence to understand the full relationship between GI problems and MCA. We know that mast cells have the capacity to release chemical inflammatory mediators including; histamine, leukotrienes, prostaglandins, proteases and cytokines. In the GI tract, it is possible that these mediators may be affecting smooth muscle contraction (to increase or slow the propulsion of food through the GI tract) and may increase leakiness and mucus secretion (to cause more watery-type diarrhea). But understanding how MCA works in patients to cause symptoms requires further research.
An improved understanding of MCA is critical because it appears to be more common than initially thought. MCA is now implicated in many chronic medical conditions such as Irritable Bowel Syndrome (IBS), Fibromyalgia and Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS). Overlapping symptoms in these disorders may be attributable to MCA because of the diverse array of mast cell mediators that may be involved and that act on multiple organ systems. Although it will be hard to determine how many patients suffer from disorders due to abnormal MCA, it is likely that all physicians see at least a handful of these patients in their practices. MCA may be playing a role in as much as 15-20% of the patient population who have chronic, multi-system symptoms. This is hypothesized based on what we know about mast cell biology in relation to inflammatory disorders.

DIAGNOSIS
Although we would like to think that physicians at the local level increasingly recognize MCAD, the reality is that many do not consider these disorders when confronted with a patient presenting with multiple seemingly unrelated complaints. Like dysautonomia patients, mast cell patients present heterogeneously with complaints that may differ from patient to patient. This makes it difficult for doctors to recognize and diagnose such conditions. For this reason, it is important that patients be proactive and educate physicians about their suspected condition(s) and even help them understand which tests are needed to make a diagnosis. A wealth of information is available on The Mastocytosis Society website (www.tmsforacure.org). In the case of MCAS, much of the diagnosis still relies on the physician’s ability to elicit the key signs and symptoms of MCA and to ensure that there is no other condition that better explains the patient’s symptom profile. The physician must also determine whether a patient has adequately responded to anti-mast cell mediator medications, which support the mast cell activation diagnosis. Lab tests are used to confirm the diagnosis. Since some lab tests are more or less specific for detecting abnormal mast cell activation and many variables have the potential to interfere with consistent findings more research is needed to improve and standardize laboratory tests. Most tests are sent out to various labs in the country such as Mayo Clinic so any physician can order them. Common screening tests used at Brigham and Women’s Hospital for MCAS are a serum tryptase, a 24 hour urine for N-methyl histamine, prostaglandin D2 or its metabolite 11-beta prostaglandin-F2α. Although urine samples must be kept refrigerated until submitted to the laboratory (unless your lab provides collection bottles with chemicals added to stabilize the sample without refrigeration) these metabolites are thought to be relatively stable. These tests are ideally performed when the patient is at their “baseline” and then repeated during a flare of symptoms or during the acute onset of symptoms. If a clonal mast cell disorder such as systemic mastocytosis is suspected because of an elevated tryptase, characteristic urticaria pigmentosa rash, a history of unexplained anaphylaxis, or other clinical features, then a KIT D816V mutation can be screened for with a blood test. It is recommended that a specialist with knowledge of these disorders sees the patient with a strongly suspected or confirmed MCAD. Consultation with an experienced specialist will help confirm the diagnosis, characterize it among the spectrum of mast cell disorders and determine whether a patient will need additional testing such as a bone marrow examination, colonoscopy with biopsies, or a bone DEXA scan.
GASTROINTESTINAL FINDINGS
The three most common GI symptoms that accompany MCAD and dysautonomia are:
Abdominal Pain
(Some component of this is seen in nearly all MCAD patients. Note: this is also common in many primary GI disorders such as IBS).
Diarrhea
Bloating and gas
Additional GI complaints include: constipation, gastroparesis (slow emptying of the stomach), nausea, vomiting, and gastroesophageal reflux disease (aka “GERD”) that may result in heartburn and occasional swallowing difficulties.
When patients are evaluated for the above GI symptoms, health care providers often consider and rule out other inflammatory conditions such as celiac disease, inflammatory bowel disease (ulcerative colitis, Crohn’s disease, microscopic colitis), chronic infections (such as Giardia), malignancy (colon cancer), and functional GI disorders such as IBS where there is no obvious abnormality detected on testing. It is important to note that many of these disorders may present with similar symptoms so specific testing may be required to differentiate them.

A key clue that a patient may have a mast cell disorder is the presence of complaints and ongoing symptoms in many organ systems (GI tract, skin, lungs) of varying severity and intensity.
These other symptoms outside of the GI tract may include fatigue, flushing, dermatographism, memory/concentration difficulties, headaches, itching and respiratory problems. Symptoms tend to wax and wane and may be triggered by various environmental factors such as certain foods, temperature changes, bites/stings, stress and strong inhaled scents. When present with dysautonomia it is common to have orthostatic issues (symptoms such as light-headedness and palpitations upon standing), peripheral neuropathies (numbness and tingling in the feet and/or hands), GI issues that sometimes include the upper GI tract including gastroparesis, reflux, and nausea. These complaints associated with MCA appear to be fairly prevalent in the dysautonomia population and especially in patients with POTS.
Since many Gastroenterologists would likely not consider dysautonomia and/or MCAD when assessing a patient’s GI symptoms, two-way communication between patient and physician is often a crucial element in the diagnostic process. Ultimately, the process of diagnosing MCAD may be lengthy and time consuming. It is important that both patient and physician are diligent and that patients strive towards the detection of objective findings that can validate the suspected condition. Although this diagnostic process may be frustrating to the patient, having a high suspicion for a mast cell disorder is a valuable first step.
Recommendations:
Rule out Dysautonomia
Once a mast cell disorder has been identified, it may be helpful to evaluate for the co-existence of dysautonomia due to the observed possible association of these disorders. This can be done initially in the clinic by assessing the orthostatic vital signs of the patient. If abnormal vital signs (such as a 30 beats per minute or more increase in heart rate or a drop in blood pressure of 20/10 mmHG (millimeters of mercury) after three to five minutes of standing) are identified in response to orthostatic stress, a full autonomic workup by a knowledgeable dysautonomia specialist may be warranted. A number of reputable autonomic specialists can be found on the www.DysautonomiaInternational.org or DINET.org websites. It is important to recognize the presence of dysfunction of the ANS in order to provide a complete set of treatment options for the patient.
Find an Effective Local Doctor
Perhaps in no other medical condition is it more important to have good two-way communication between the patient and physician than in the case of MCAD. This is because the medical community is still learning about the pathophysiology of MCA and associated disorders. Further, the dissemination of clinical research findings often do not make their way down the chain quickly to the local treating physician. Finding an effective local doctor means finding a physician who is willing to work with an out of town specialist, refer to appropriate specialists and learn about MCAD and/or dysautonomia themselves. Effective continuity and communication between the local physician, specialist, and patient is necessary for optimal clinical outcomes.
Patient Education and Advocacy
Patient education about MCA disorders and/or dysautonomia is helpful in both developing knowledge about these conditions so as to arrive at the appropriate diagnosis and to seek the best treatments. Further, the patient or family caregiver is often the best advocate in dealing with various providers, hospitals and emergency care centers.
Below is a list of learning points for both patient education and advocacy:
Mast cells are protective in nature.
They act much like soldiers with ammunition made of chemical mediators (histamines, prostaglandins, leukotrienes, and other cytokines) that when working properly help to fight off various invaders of the body such as bacteria, viruses, parasites, toxins, etc. However, there are several disorders where these mast cells activate abnormally leading to the inappropriate release of chemical mediators that can play havoc in many and/or all organ systems.
Mast cells are a key player in the immune system.
In MCAD, the mast cell abnormally activates releasing the chemical components, which have a direct effect on symptoms within the body including vasodilation (effects on blood vessels that may result in symptoms such as flushing or light-headedness with standing) and inflammation. Since mast cells inappropriately activate in close proximity to the nerves, which are located in multiple organ systems throughout the body, it is not a surprise that patients may have multi-organ symptoms, neuropathies, potential autonomic dysfunction and other nerve symptoms throughout the body. It is important to note that there is not sufficient evidence that MCADs are auto-immune in nature. In autoimmune disease the immune system attacks itself in one or more localized region(s) of the body. In such conditions mast cells play more of an accessory role rather than a direct role in contributing to localized inflammation. Instead, in MCAD, it may be helpful to think of the mast cells as being abnormally overactive or hyper-immune.
Mast Cell Activation Disorders Can Be Managed.
Although there is no known cure for MCAD, most patients with indolent (benign) systemic mastocytosis can expect a near normal life expectancy if they are diagnosed and managed correctly, avoid triggers, and are always cognizant that they are at increased risk of anaphylaxis. Nonetheless, MCAD can cause chronic and acute symptoms that may be chronically disabling in nature (poor quality of life, loss time from work, hospitalizations, unnecessary medical procedures and interventions). The ideal treatment addresses the “whole patient” and not just one organ system at a time (See below for recommended pharmacological treatments). The overall management should include pharmacological and non-pharmacological treatments.
Knowledgeable Mast Cell Activation Patients Are Advocates.
Since MCAD patients present heterogeneously, it is crucial that the patient and/or caregiver are knowledgeable and seek to gather clinical data regarding their specific case. The following are helpful items for patients to keep in mind. Keep important medical records including consultation notes, and the results of diagnostic tests, laboratory tests, and radiology studies. Know which triggers affect your symptoms, especially what foods or environmental factors (for example scents, paints, pollen, dust, and pets). It may be helpful to keep a detailed food diary including not just what was eaten but specifically how it was prepared (such as white bread toasted with butter and honey). Use data to track and identify symptom trends. It is helpful to keep a symptom log to record and identify trends, particularly the constellation of symptoms that may constitute a flare. Learn which treatments are most helpful including regular maintenance treatments and those treatments that are helpful when breakthrough and/or acute symptoms occur. It is also helpful to keep a list of which treatments have been tried previously and why they were discontinued. Allergies and intolerances to all medications should be listed. It requires patience and persistence when trying new medical treatments. Your doctor may tell you to start a medication at a lower dosage and titrate to maximal affect. The risks and benefits of continuing with a medication that may cause side effects should be discussed with your provider.
Treatments
There are many options to consider when adopting a treatment regimen to manage the GI issues associated with MCA disorders and dysautonomia. There is no one standard approach and the regimen should be individualized to optimally treat symptoms and any co-existing conditions. In general, the pharmacological treatments either stabilize or inhibit the activation of mast cells or inhibit the effect of the specific chemical mediators that mast cells release. The cornerstone of treatment is to avoid known triggers of symptoms. Along these lines, the selection of an appropriate diet is essential to the management of GI symptoms. While specific foods should be avoided that provoke symptoms, the diet must be properly balanced to maintain proper nutrition and enhance health (see below). Patients should seek a healthy lifestyle in general that includes regular exercise (or movement to avoid deconditioning), appropriate coping mechanisms, and social support systems.
The following table may be used as a guide to identify appropriate pharmacological treatments. Medications are often added starting from the top of the list and proceeding down in a step-wise manner. Any medical regimen should be discussed first with the treating physician.

* Halmos EP et al, Gastroenterology 2014 Jan;146(1)
Research Creates Hope for the Future
Hope for the future is dependent upon further research that will enhance our understanding of the pathophysiology, genetic predispositions and effective mechanisms for preventing and remediating conditions involving MCAD and dysautonomias with co-existing GI symptoms. The following are key research areas that have been identified and relevant barriers, which may stand in the way.
There is a great need for improved diagnostics. Although there are clear diagnostic criteria that have been used over decades for Systemic Mastocytosis and Mast Cell Leukemia, more objective and accessible criteria are needed for MCAS. Although the members of The Mastocytosis Society Medical Advisory Board and other members of the medical community have worked diligently in recent years to define consensus statements regarding the diagnosis of MCAS, there remains wide variation in criteria used (for example whether or not a positive test for a mast cell mediator constitutes MCA and whether this should be tested at baseline or during a flare). There is also the difficulty that these criteria may not be accurate enough to detect MCA in a certain individual at a certain time. Since assuring an accurate diagnosis is essential for providing meaningful treatment and not to miss other important diagnoses, progress in this area of study is crucial as more patients and physicians learn about MCAD.

As research in the areas of GI and MCA emerge there needs to be an emphasis on the genetic factors that may predispose people to MCAD. This will be able to help patients with the diagnosis, prognosis, and treatment of their disease. In addition, it will be important to develop better ways to phenotype patients with MCAD. In MCAS, this may include the study of different protease expressions within an individual in the various organ tissues, whether or not a patient has a history of anaphylaxis, and which mast cell mediators are abnormally elevated and how this may correlate with specific symptoms or response to therapies.
Currently, there is a great divide amongst researchers studying dysfunction of the autonomic nervous system and those studying mast cell disorders. Often easy to assess diagnostic data such as orthostatic vital signs are overlooked by mast cell disorder specialists. Conversely, information reported in the patient history (such as a history of anaphylaxis, flushing, multi-organ system dysfunction and abdominal pain) that may require an MCAD workup is often overlooked.
Nutritional studies are difficult and often avoided by researchers for many reasons including the difficulty in defining meaningful criteria, poor compliance, poor patient recall and the need for full control over the diet. Nonetheless such studies would be helpful to provide scientific evidence to support the use of dietary interventions as a mainstay of treatment for MCAD.
Funding research has always been difficult. Now, more than ever, as NIH budgets decrease, the need for private funding and partnering with other organizations, even other countries, is clear. When writing research proposals in the United States, it is often helpful to pair the research need with a well known condition such as diabetes, heart disease and/or cancer. Often grant proposals, which focus on the lesser known or rare disorders, are rejected, as they don’t appear, at first glance, to meet the needs of a large patient population. Building collaborations to spread out available funding and resources will be important to continue funding this research.
Patients play a key role in advancing research. There are the traditional means for supporting research including participating in/or leading fundraisers for private organizations that fund research and writing to leaders who govern state and federal research funding. But often patients underestimate the power they have in creating awareness by educating friends, family and even their own physicians who are the leaders in advancing such clinical research. All patients who suffer with mast cell disorders (especially those whose cases are life threatening and/or complicated with dysautonomia and difficult GI issues) will benefit with greater understanding within these areas of research. It is this greater understanding that gives us all “hope for the future”.
Written by Kelly Freeman, M.S.M. and Matthew J. Hamilton, M.D. Reviewed and edited by Satish Raj, M.D., Valerie Slee, B.S.N., Susan Jennings, Ph.D., and Nancy Russell, Dr. PH.
Matthew J. Hamilton, M.D. practices in the Division of Gastroenterology and is active in research in the Mastocytosis Center for Excellence at Brigham and Women’s Hospital. He is also a faculty member at Harvard Medical School.
Kelly Freeman, M.S.M. is the Founding Director for TheDysautonomiaProject.org She has several years of experience in health care education and research.
































2 Responses
Hi Kelly.
Just wondering whether the air hunger i get when i take any antibiotics or other meds is a mast cell degranulation going on in lung or in vasculature or whether the medications set off dysautonomia/dyfunctional breathing somehow.
Im desperately trying to find answers as i also carry Braca 1 gene and need lots of life saving surgeries but cant tollerate antibiotics, anaestetics or painkillers. Really dont know where to turn.
Sorry to disturb you. 😌
Susan, My apologies for a delayed reply. The answer to your question is it may be. We need more information to know. Air hunger is also very common among patients with autonomic disorders. In most cases the cause is unknown. There was some new research done last year at UNC Pembroke about this prevalence. In MCAS patients are prone to having reactions to many medications so you are not alone. It is helpful to work with an immunologist or MCAS specialist to determine what alternative medications may be helpful. -K